While it sometimes feels like the COVID years are behind us, and that perhaps some of the trauma from lockdowns are beginning to heal, the truth is that many of the changes made, and much of the trauma endured by our society are here to stay. The pandemic has had an indelible impact on our society, even for those who have never been sick. For the majority of people that have been sick with COVID, there can also be troubling prolonged symptoms that persist long past a negative test.
Despite less severe cases, positive tests are still canceling parties, and plans are still being rearranged due to the onset of the common cold. After all, could it be more than a cold? It can take a few days to test positive, so it is hard to know! What’s worse is that Long COVID symptoms are affecting up to 80% of the population for some period of time after testing negative. It is occurring in both those who have been infected by COVID, and in some after vaccination, or their latest booster.
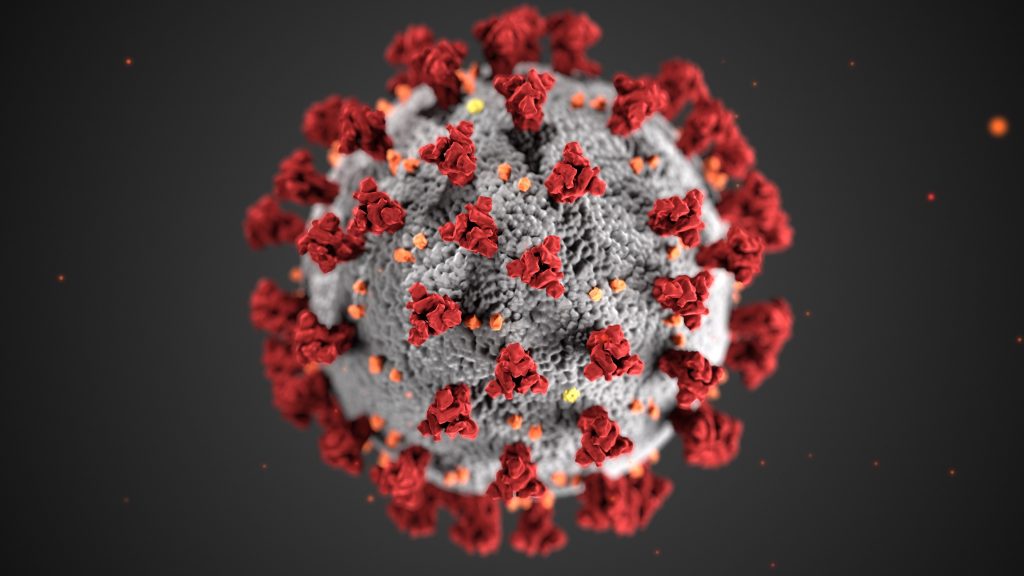
Though researchers are actively studying long COVID, we don’t yet have a full understanding of all of the mechanisms behind it, because it affects people so differently, but there are many theories emerging. One possibility is that symptoms are due to the monocyte/microglia activation by the spike protein that comes from the virus as well as from the vaccine. This results in an ongoing inflammatory response in an attempt by the immune system to clear the offending proteins and viral RNA fragments.
Many Long COVID sufferers are finding their way to Functional Medicine for relief, because a full work-up often reveals long-standing deficiencies, gut issues, inflammation, hormone imbalances, and more that had not affected their health until the virus preyed on these underlying weaknesses. Long COVID is a very troubling condition for sufferers and their loved ones alike, as there are still so many unknowns, and the symptoms can be debilitating.

What is Long COVID?
Long COVID, also known as Long Haul COVID Syndrome (LHCS), refers to symptoms experienced by patients after the acute symptoms of a COVID-19 infection have dissipated. Symptoms of Long COVID are wide-ranging and some people do not even know that their new chronic health issues actually stemmed from having had the infection or vaccine.
People experience prolonged malaise/body aches, headaches or migraines, generalized fatigue, sleep difficulties, increased anxiety, hair loss, smell disorder, decreased appetite, painful joints, dyspnea/trouble breathing, chest pain, heart palpitations, and brain fog. There can also be prolonged neuropsychological symptoms that affect multiple domains of cognition and memory.
Latent viral or bacterial infections can be reactivated, like Epstein Barr virus, Herpes, or even chronic Lyme’s disease, leading to overall immune suppression and a host of other varied symptoms.
Some people experience severe symptoms, while others have milder symptoms, but they are all difficult to treat with conventional medicine, as there is not one specific underlying cause for all cases. Another interesting fact about Long COVID is that the severity of symptoms is NOT related to the severity of the initial COVID infection. One could have a mild case of COVID-19 and end up with debilitating Long COVID symptoms!
How do I know if I have Long COVID?
If you are experiencing persistent symptoms after a bout with a COVID infection, begin documenting your symptoms daily. Make an appointment with your doctor and share your symptoms log. Get a full work up to look for underlying vitamin deficiencies, reactivated viruses, hormone dysfunction, and other imbalances that can lead to these prolonged symptoms.
Though there isn’t a test to confirm a long COVID diagnosis, your physician will be able to assess your symptoms and your personal medical history to determine if a long COVID diagnosis is appropriate. You may also be referred to specialists, depending on the nature of your symptoms. By keeping your symptom log current, you’ll be able to give each provider a clear picture of your experience.
Similar symptoms are being reported after doses of the vaccine as well, and it is likely due to a similar process from excess spike protein buildup in the body. It seems that the same treatments of detoxing the spike protein, decreasing inflammation, optimizing underlying weaknesses, and boosting the immune system also work for the symptoms from the vaccine as well.
I have Long COVID. Now what?
If you have been diagnosed with Long COVID, you may feel both relief and frustration. While you might be relieved to receive a specific diagnosis, you might also feel overwhelmed, especially because there is no way to know if your symptoms will last for a few weeks, months, or even years.
While there is no one-size-fits-all cure for Long COVID, and conventional treatments are often geared at medicating specific symptoms, there are often underlying weaknesses that need to be identified and treated.
Make an appointment with a functional medicine doctor and share your symptoms log. Get a full work up to look for underlying vitamin deficiencies, reactivated viruses, hormone dysfunction, and other imbalances that can be the underlying cause of these prolonged symptoms. Once these individual weaknesses have been identified and corrected, inflammation can be reduced, the immune system can bounce back, and the body can more easily clear viral particles and spike protein.

Find strength in numbers
After getting a diagnosis and having a work-up to look for underlying weaknesses that could be the root of the symptoms, connecting to other long COVID sufferers can also be a source of strength. By regularly meeting with other people with long COVID, you feel less alone. Group meetings can offer many benefits. Within the group, you can share experiences, frustrations, and tips for creative ways to manage stress, as stress and exertion often exacerbate symptoms. Sometimes you just need a space to vent about your frustrations dealing with your lingering illness! You can learn a lot from the experience others have had with long COVID – what could be hidden triggers, what makes things worse, or better? Consider finding a like-minded group to connect with about this disease.
Look for a group led by a medical professional who will guide the testing, the protocols, the diet, and teach you what you need to do to decrease inflammation and boost your immune system in the correct way! Find someone who will serve as a resource for reliable information about long COVID, as the information is changing rapidly as more time passes and more people suffer from lingering symptoms.
If you’re suffering from long COVID and looking for a community where you can share your concerns, help is available if you are in Colorado, Georgia or California.
Due to the overwhelming prevalence of Long COVID and vaccine side effects, Golden Road Medicine has started offering a functional medicine group model to help identify underlying common deficiencies and imbalances underlying the symptoms. There is a one-on-one personalized intake with the doctor, lab work ordered for each patient, group lab work reviews, successful supplementation protocols shared, a spike protein anti-inflammatory detox diet, advice on lowering inflammation, balancing hormones and much more in our 12-week Long COVID program. You also get that great and much needed group support while you heal.
Click here for more information about the Long COVID treatment groups. If you have any questions after learning more, book a free ten-minute consultation with Dr. Courtney King, to see if it is right for you.